If you’re reading this because you’re in pain that doctors keep dismissing as “normal,” you’re not alone. I spent years being told my excruciating periods were just part of being a woman, until I finally got answers.
What is endometriosis? It’s a condition where tissue similar to your uterine lining grows outside your uterus, causing severe pain, inflammation, and potentially fertility issues. But more than that medical definition, endometriosis is often a journey of being dismissed, gaslit, and told your pain isn’t real.
I know because I lived it. From teenage years laying on bathroom floors in agony to giving up university dreams because of daily pain, endometriosis affects 1 in 10 women of reproductive age, yet takes an average of 7-12 years to diagnose.
What Is Endometriosis Really Like to Live With?
When people ask “what is endometriosis,” they usually want the textbook definition. But let me tell you what endometriosis actually feels like.
It’s 1000/10 pain that makes you curl up wherever you are – the bathroom floor, your bed, the couch. It’s missing school, work, and life because the pain is simply unbearable. It’s being told by doctor after doctor that this level of suffering is “normal” for women.
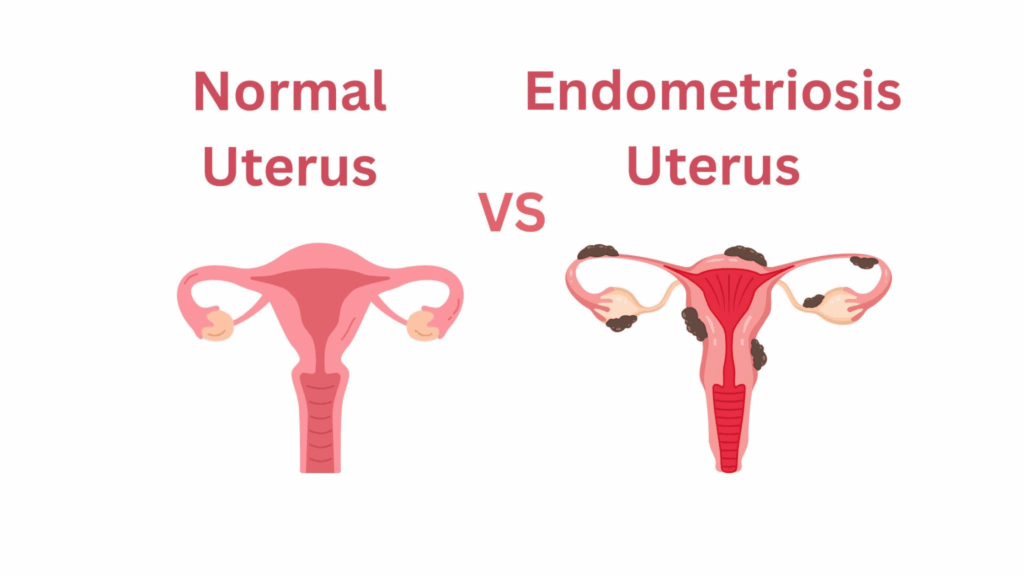
The medical definition of endometriosis is that it occurs when endometrial-like tissue (but not the same tissue) grows outside the uterus, commonly on the ovaries, fallopian tubes, and pelvic lining. This tissue behaves like your normal uterine lining – it thickens, breaks down, and bleeds with each menstrual cycle. But unlike your period blood, this has nowhere to go, causing inflammation, scar tissue, and adhesions.
It’s a condition that can steal years of your life while you search for answers.
Why Do So Many Doctors Miss the Signs? What Is Endometriosis Misdiagnosed As?
Many healthcare providers still don’t recognize endometriosis symptoms or take women’s pain seriously. During my journey, I was told my pain was:
- Normal period pain
- Stress from university
- “All in my head”
- Something I needed to manage with painkillers
- IBS or digestive issues
Studies show that medical professionals often dismiss women’s pain, and endometriosis symptoms overlap with many other conditions.
Common misdiagnoses include:
| Condition | Why It’s Confused with Endometriosis |
| IBS | Digestive symptoms, bloating, pain with bowel movements |
| Appendicitis | Right-sided pelvic pain |
| Ovarian cysts | Pelvic pain, irregular periods |
| PID | Pelvic pain, painful intercourse |
| “Normal” period pain | Severe menstrual cramps dismissed as typical |
“I went to so many gastroenterologists, but no one helped. They all said it was stress from uni, that it was in my head, and there’s nothing wrong with me as all my medical exams are normal.” – Ivana Soldat
What Are the Real Symptoms of Endometriosis? (Beyond Just Painful Periods)
What is endometriosis like symptom-wise? It’s so much more than just bad periods.
Here are the signs that something might be seriously wrong:
During Your Period:
- Pain so severe you can’t function (not just “uncomfortable”)
- Pain that doesn’t respond to over-the-counter painkillers
- Having to miss work, school, or important events
- Nausea and vomiting from pain intensity
- Heavy bleeding or irregular periods
Beyond Your Period:
- Painful sex (dyspareunia) – This was my second red flag, but I was too embarrassed as a teenager to mention it
- Daily pelvic pain – Not just during periods, but constant aching or cramping
- Bathroom problems – Pain when urinating or having bowel movements
- Digestive issues – Bloating, constipation, or diarrhea, especially during periods
- Fatigue – Exhaustion that goes beyond normal tiredness
- Fertility struggles – Difficulty getting pregnant
The Emotional Symptoms:
- Anxiety and depression from chronic pain
- Feeling isolated and misunderstood
- Frustration from medical dismissal
- Fear that you’re “going crazy” or imagining symptoms
How Is Endometriosis Diagnosed?
There’s no simple blood test for endometriosis. The gold standard for diagnosis is laparoscopy – a minimally invasive surgical procedure where a tiny camera examines your pelvic organs.
The Diagnostic Journey:
Step 1: Finding the Right Doctor
Not all gynecologists are endometriosis specialists.
Look for:
- Reproductive endocrinologists
- Minimally invasive gynecologic surgeons (MIGS)
- Doctors specifically trained in endometriosis
Step 2: Medical History and Physical Exam
A good doctor will:
- Take your pain seriously (red flag if they dismiss it)
- Ask detailed questions about your symptoms
- Perform a pelvic exam (may be painful if you have endometriosis)
- Listen to your complete story without interrupting
Step 3: Imaging Studies
- Pelvic ultrasound – Can detect ovarian cysts and some forms of endometriosis
- MRI – Better at showing deep infiltrating endometriosis
- Advanced ultrasound protocols – Some centers have specialized endometriosis imaging
Step 4: Laparoscopic Surgery
- The only definitive way to diagnose endometriosis
- Tissue samples are examined under microscope
- Usually day surgery with small incisions
How Many Stages of Endometriosis Are There?
Once diagnosed, endometriosis is staged from I-IV:
- Stage I (Minimal) – Few small implants
- Stage II (Mild) – More implants, some deeper
- Stage III (Moderate) – Many implants, some cysts, adhesions
- Stage IV (Severe) – Extensive implants, large cysts, significant adhesions
Important note: Stage doesn’t always correlate with pain level. You can have Stage I and be in excruciating pain.
What Treatment Can Help With Endometriosis?
After getting my diagnosis in November 2024, I learned that treatment is highly individual. But the treatment really depends on your symptoms, age, and fertility goals.
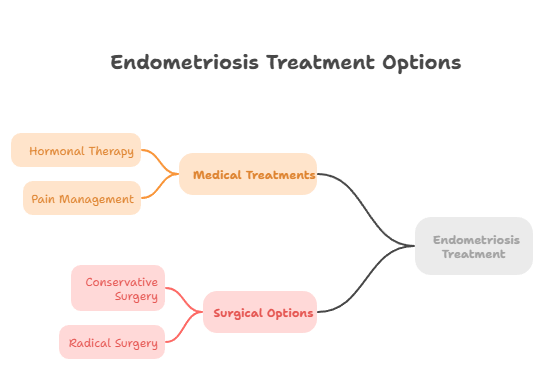
Medical Treatments:
Hormonal Therapy:
- Birth control pills (continuous use)
- Progestin therapy
- GnRH agonists (medical menopause) – This is what I’m currently trying
- Aromatase inhibitors
Pain Management:
- NSAIDs (though often insufficient alone)
- Prescription pain medications
- Nerve blocks for severe cases
Surgical Options:
Conservative Surgery (Laparoscopy):
- Removes endometriosis implants
- Preserves reproductive organs
- Can provide significant pain relief
- May need to be repeated
Radical Surgery (Hysterectomy):
- Only for severe cases
- May include ovary removal
- Not guaranteed to cure endometriosis
- Major decision, especially for young women
Living with Endometriosis: What Does Daily Life Look Like?
What is endometriosis like day-to-day? Honestly, it’s like living with an unpredictable roommate who decides when you can and can’t function. Some mornings I wake up feeling almost normal, and others I can barely get out of bed because of the pain.
Finding What Works for Pain Management
Over the years, I’ve discovered that my heating pad has become my best friend. I’m curled up with a hot water bottle 24/7. When I’m having a decent day, I try to do as much as I can around the house, even though it often results in me needing to have a 24 hour rest after, but at least my mind is a bit clearer. I’ve learned that my body speaks a different language than it used to, and I’m still learning to listen.
Stress makes everything worse, which is frustrating because having chronic pain is inherently stressful. I’ve had to get creative with managing this vicious cycle. Sometimes it’s deep breathing exercises, sometimes it’s just allowing myself to feel all the emotions. Or just thinking that all is well and there’s no need to stress.
Building a support network has been crucial, though it took time to figure out who truly understood and who just offered empty platitudes.
Becoming Your Own Medical Advocate
This part has been both empowering and exhausting. I keep detailed symptom diaries now. Not because I enjoy documenting my misery, but because it’s the only way doctors take me seriously. I try to track most things: pain levels, what I ate, when pain peaked, etc. It feels obsessive sometimes, but it’s given me adrenaline to fight back when doctors try to dismiss my concerns.
I’ve learned to research specialists obsessively before appointments. After years of being told my pain was “normal” or that I should just take paracetamol, I refuse to accept inadequate care.
I come prepared with questions, and I don’t leave until I get real answers. My husband has started coming to all appointments with me because having a witness somehow makes doctors listen more carefully.
Protecting Your Mental Health
When I mention considering counseling, it’s not because this is “all in your head.” Trust me, I’ve heard that enough for several lifetimes. It’s because living with chronic pain genuinely affects your mental health, and you deserve support for that. I went to therapy for over a year, not to cure my endometriosis, but to learn how to cope with the emotional toll it takes.
Connecting with other women who have endometriosis has been life-changing. Online support groups, even just finding one person who truly gets it – these connections remind you that you’re not crazy, you’re not weak, and you’re definitely not alone.
On my worst pain days, I practice what I call aggressive self-compassion. Instead of beating myself up for canceling plans or calling in sick, I remind myself that I’m dealing with a real, documented medical condition.
I’ve also had to educate my family and friends about endometriosis, which has been an ongoing process. Some people get it immediately, others need repeated explanations, and unfortunately, some never will. Learning to let go of the people who refuse to understand has been hard but necessary for my peace of mind.
How to Advocate for Yourself
Based on my journey from Croatia to Italy, searching for doctors who’d listen, here’s how to advocate for yourself:
Red Flags in Healthcare Providers:
- Dismissing your pain as “normal”
- Refusing to order tests or referrals
- Saying “it’s all in your head”
- Not examining you thoroughly
- Rushing through appointments
Green Flags in Healthcare Providers:
- Taking detailed symptom history
- Validating your pain experience
- Explaining all testing options
- Referring to specialists when needed
- Reading through your previous medical records
Questions to Ask Your Doctor:
- “Could my symptoms be endometriosis?”
- “What tests can rule out or confirm endometriosis?”
- “Can you refer me to an endometriosis specialist?”
- “What are all my treatment options?”
- “How will this affect my fertility?”
The Hope After Diagnosis
Getting diagnosed with endometriosis isn’t the end of your journey. It’s a new beginning of getting real help. While there’s no cure, many women find significant relief through proper treatment.
You are not alone. Your pain is real. Your symptoms matter. And you deserve healthcare providers who believe you and want to help.
If you have been struggling to get an endometriosis diagnosis, share your story in the comments below. Your experience might help another woman realize she’s not alone in this journey.
This article combines personal experience with current medical research on endometriosis diagnosis and treatment. Always consult with healthcare professionals for personalized medical advice.